What Is Spinal Fusion?(when is it necessary?)
Spinal fusion is surgery to join two or more vertebrae into one single structure. The goal is to stop movement between the two bones and prevent back pain. Once they’re fused, they no longer move like they used to. This keeps you from stretching nearby nerves, ligaments, and muscles that may have caused discomfort.
why is spinal fusion done?
 Spinal fusion permanently connects two or more vertebrae in your spine to improve stability, correct a deformity or reduce pain. Your doctor may recommend spinal fusion to treat the following spine problems:
Spinal fusion permanently connects two or more vertebrae in your spine to improve stability, correct a deformity or reduce pain. Your doctor may recommend spinal fusion to treat the following spine problems:
- Broken vertebrae:Not all broken vertebrae require spinal fusion. Many heal without treatment. But if a broken vertebra makes your spinal column unstable, spinal fusion surgery may be necessary.
- Deformities of the spine:Spinal fusion can help correct spinal deformities, such as a sideways curvature of the spine (scoliosis) or abnormal rounding of the upper spine (kyphosis).
- Spinal weakness or instability:Your spine may become unstable if there's abnormal or excessive motion between two vertebrae. This is a common side effect of severe arthritis in the spine. Spinal fusion can be used to restore spinal stability in such cases.
- Spondylolisthesis:In this spinal disorder, one vertebra slips forward and onto the vertebra below it. Spinal fusion may be needed to treat spondylolisthesis if the condition causes severe back pain or nerve crowding that produces leg pain or numbness.
- Herniated disk:Spinal fusion may be used to stabilize the spine after removal of a damaged (herniated) disk.
The surgical decision
If you are a candidate for spinal fusion, the surgeon will explain your options. Consider all the risks and benefits as you make your decision. Fusion is performed only after other treatments have been explored. It will stop the motion in the painful area of your spine, allowing increased function and return to a more normal lifestyle—though one that may not be totally pain-free. Your surgeon will also explain the various types of bone graft. These materials are placed within the remaining disc space and act as a kind of mortar between the bones as your body heals. Each type has advantages and disadvantages.
- Autograft is your living bone. The marrow contains bone-growing proteins. It can be collected from drillings during the surgery or taken from the hip as an iliac crest bone graft. The harvested bone is about a half inch thick. The entire thickness of bone is not removed
- BMA (bone marrow aspirate) is your living bone marrow, collected with a syringe from the hip (iliac bone) or vertebra. It is relatively painless compared to an iliac crest graft.
- Allograft is bone from an organ donor, collected and stored by a bone bank. The donor graft has no bone-growing cells.
- BMP (bone morphogenetic protein) is sometimes added to bone-graft material to stimulate bone growth naturally in the body.
Who performs the Spinal fusion procedure?
A neurosurgeon or orthopedic surgeon can perform spine surgery. Many spine surgeons have specialized training in minimally invasive surgery. Certain minimally invasive techniques are highly technical; they require special instruments and training to avoid complications. Ask your surgeon about his or her training, especially if your case is complex or you have had previous spinal surgery.
What happens before Spinal fusion?
 Presurgical tests (e.g., blood test, chest x-ray, electrocardiogram) will be done several days before surgery. In the doctor's office, you will sign consent forms and provide your medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, previous surgeries). Inform your healthcare provider about all the medications (over-the-counter, prescription, herbal supplements) that you are taking. Continue taking the medications your surgeon recommends. Stop taking all non-steroidal anti-inflammatory medicines (Naprosyn, Advil, Motrin, Nuprin, Aleve, etc.) and blood thinners (Coumadin, Plavix, etc.) 1 to 2 weeks before surgery as directed by your doctor. Ask your doctor if you are unsure. Stop smoking before surgery. The most important way to achieve a successful spine fusion is to eliminate tobacco use (cigarettes, cigars, pipes, chewing tobacco) before surgery. Nicotine prevents bone growth and decreases successful fusion. Smoking risk is serious: fusion fails in 40% of smokers compared with 8% of non-smokers. Smoking also decreases blood circulation, resulting in slower wound healing and increased risk of infection.
Presurgical tests (e.g., blood test, chest x-ray, electrocardiogram) will be done several days before surgery. In the doctor's office, you will sign consent forms and provide your medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, previous surgeries). Inform your healthcare provider about all the medications (over-the-counter, prescription, herbal supplements) that you are taking. Continue taking the medications your surgeon recommends. Stop taking all non-steroidal anti-inflammatory medicines (Naprosyn, Advil, Motrin, Nuprin, Aleve, etc.) and blood thinners (Coumadin, Plavix, etc.) 1 to 2 weeks before surgery as directed by your doctor. Ask your doctor if you are unsure. Stop smoking before surgery. The most important way to achieve a successful spine fusion is to eliminate tobacco use (cigarettes, cigars, pipes, chewing tobacco) before surgery. Nicotine prevents bone growth and decreases successful fusion. Smoking risk is serious: fusion fails in 40% of smokers compared with 8% of non-smokers. Smoking also decreases blood circulation, resulting in slower wound healing and increased risk of infection.
Morning of surgery
- No food or drink.
- Shower using antibacterial soap. Dress in freshly washed, loose-fitting clothing.
- Wear flat-heeled shoes with closed backs.
- If you have instructions to take regular medication the morning of surgery, do so with small sips of water.
- Remove make-up, hairpins, contacts, body piercings, etc.
- Leave all valuables and jewelry at home.
- Bring a list of medications (prescriptions, over-the-counter, and herbal supplements) with dosages and the times of day usually taken.
- Bring a list of allergies to medication or foods.
- Arrive at the hospital 2 hours before (outpatient surgery center 1 hour before) your scheduled operation to complete the necessary paperwork and pre-procedure work-ups. An anesthesiologist will talk with you and explain the effects of anesthesia and its risks. An intravenous (IV) line will be placed in your arm.
During spinal fusion
 Surgeons perform spinal fusion while you're under general anesthesia so you're unconscious during the procedure. Surgeons have developed a variety of techniques for performing spinal fusion surgery. The technique your surgeon uses depends on the location of the vertebrae to be fused and the reason for the spinal fusion. Generally, the procedure involves the following:
Surgeons perform spinal fusion while you're under general anesthesia so you're unconscious during the procedure. Surgeons have developed a variety of techniques for performing spinal fusion surgery. The technique your surgeon uses depends on the location of the vertebrae to be fused and the reason for the spinal fusion. Generally, the procedure involves the following:
- Incision: To gain access to the vertebrae being fused, the surgeon makes an incision in one of three locations: in your neck or back directly over your spine, on either side of your spine, or in your abdomen or throat so that your surgeon can access the spine from the front.
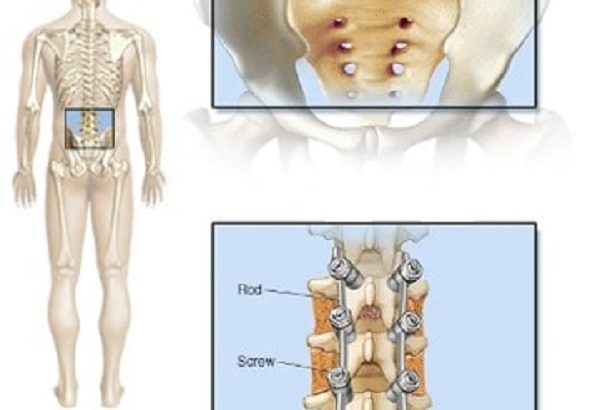
- Bone graft preparation: The bone grafts that actually fuse two vertebrae together may come from a bone bank or from your own body, usually from your pelvis. If your own bone is used, the surgeon makes an incision above your pelvic bone, removes a small portion of it and then closes the incision.
- Fusion: To fuse the vertebrae together permanently, the surgeon places the bone graft material between the vertebrae. Metal plates, screws or rods may be used to help hold the vertebrae together while the bone graft heals.
In selected cases, some surgeons use a synthetic substance instead of bone grafts. These synthetic substances help promote bone growth and speed the fusion of the vertebrae.
After spinal fusion
 A hospital stay of two to three days is usually required following spinal fusion.
A hospital stay of two to three days is usually required following spinal fusion.
Discomfort
- Do not take anti-inflammatory pain relievers (Advil, Aleve) without surgeon’s approval. They prevent new bone growth and may cause your fusion to fail.
- You may take acetaminophen (Tylenol).
- Ice your incision 3-4 times per day for 15-20 minutes to reduce pain and swelling.
Restrictions
- Avoid bending, lifting or twisting your back for the next 6 weeks.
- Do not lift anything heavier than 5 pounds for 2 weeks after surgery.
- No strenuous activity for the next 2 weeks, including yard work, housework and sex.
- DO NOT SMOKE or use nicotine products. It prevents new bone growth and may cause your fusion to fail.
- Do not drive until after your follow-up appointment. You may ride in the car for short distances of 45 minutes or less if necessary.
Activity
- You may need help with daily activities (e.g., dressing, bathing), for the first couple days.
- Get up and walk 5-10 minutes every 3-4 hours. Gradually increase your walking time, as you are able.
Bathing/Incision Care
- Wash your hands thoroughly before and after cleaning your incision to prevent infection.
- If you have Dermabond (skin glue) covering your incision, you may shower the day after surgery. Gently wash the area daily with soap and water. Pat dry.
- If you have staples, steri-strips, or stitches, you may shower 2 days after surgery. Remove the gauze dressing and gently wash the area with soap and water. Replace the dressing or completely remove it if no drainage. Inspect and wash the incision daily.
- Do not submerge or soak the incision in water (bath, pool or tub).
- Some drainage from the incision is normal. A large amount of drainage, foul smelling drainage, or drainage that is yellow or green should be reported to your surgeon’s office immediately.
- Staples, steri-strips, and stitches will be removed at your follow-up appointment.
Bracing
- If you were given a brace, wear it at all times unless you are sleeping or showering.
When to Call Your Doctor
- Call if your temperature exceeds 101.5° F. Call if the incision begins to separate or show signs of infection, such as redness, swelling, pain, or drainage.
- Swelling and tenderness in the calf of one leg.
- New onset of tingling or numbness in the legs or numbness in the groin area.
Recovery and prevention
Schedule a follow-up appointment with your surgeon for 2 weeks after surgery. Recovery time to daily activities is usually 6 to 12 weeks. X-rays may be taken after several weeks to verify that fusion is occurring. The surgeon will decide when to release you back to work at your follow-up visit. Recurrences of pain are common. The key to avoiding recurrence is prevention:
- Proper lifting techniques
- Good posture during sitting, standing, moving, and sleeping
- Appropriate exercise program
- An ergonomic work area
- Healthy weight and lean body mass
- A positive attitude and relaxation techniques (e.g., stress management)
- Healthy diet of real foods
- No smoking
Results spinal fusion
As a minimally invasive procedure, lateral lumbar fusion uses a small incision, has short operating time, minimizes blood loss, and poses few serious complications. With its minimal trauma to the spine and nearby tissues, patients often return to daily activities within 6 weeks. Each patient's result and recovery differs based on his or her health and lifestyle. Keep a positive attitude and perform your physical therapy as instructed. Achieving a spinal fusion varies depending on the technique used, your general health, and whether you smoke.
Risks Spinal fusion
Spinal fusion is generally a safe procedure. But as with any surgery, spinal fusion carries the potential risk of complications. Potential complications include:
- Infection
- Poor wound healing
- Bleeding
- Blood clots
- Injury to blood vessels or nerves in and around the spine
- Pain at the site from which the bone graft is taken
Beyond the immediate risks of the procedure, spinal fusion surgery changes how your spine works by shifting stress from the fused vertebrae to adjacent areas of your spine. This added stress may accelerate the process of wear and tear in the vertebral joints on either side of the fusion, causing further damage and possibly chronic pain.




