symptoms, treatment and surgery of Cerebral vessels’ torn and not torn Aneurysm
Brain aneurysms are often discovered when they rupture, causing bleeding into the brain or the space closely surrounding the brain called the subarachnoid space, causing a subarachnoid hemorrhage. Subarachnoid hemorrhage from a ruptured brain aneurysm can lead to a hemorrhagic stroke, brain damage and death.
The main goals of treatment once an aneurysm has ruptured are to stop the bleeding and potential permanent damage to the brain and to reduce the risk of recurrence. Unruptured brain aneurysms are sometimes treated to prevent rupture.
An aneurysm is an abnormal, weak spot on a blood vessel that causes an outward bulging or ballooning of the arterial wall. These weak spots can involve all walls of the blood vessel (fusiform aneurysm), form a sac from one wall (saccular) or separate the vessel walls (dissecting). An aneurysm can affect any vessel in the body but only those in the head can cause a serious medical condition, a hemorrhagic stroke when they rupture, which can lead to brain damage and death.
Symptoms
Ruptured Cerebral Aneurysm Symptoms
When an aneurysm ruptures, called subarachnoid hemorrhage, people often complain of "the worst headache of their life." Other ruptured cerebral aneurysm symptoms include:
- Nausea and vomiting
- Stiff neck or neck pain
- Blurred vision or double vision
- Pain above and behind the eye
- Dilated pupils
- Sensitivity to light
- Loss of sensation
Unruptured Cerebral Aneurysm Symptoms
Most aneurysms are asymptomatic, particularly ones that are small. Occasionally, large aneurysms may cause the following symptoms related to pressure on the adjacent brain or nerves:
- Peripheral vision deficits
- Thinking or processing problems
- Speech complications
- Perceptual problems
- Sudden changes in behavior
- Loss of balance and coordination
- Decreased concentration
- Short-term memory difficulty
- Fatigue
Because the symptoms of brain aneurysms can also be associated with other medical conditions, diagnostic neuroradiology is regularly used to identify both ruptured and unruptured brain aneurysms.
Diagnosis of Brain Aneurysms
Aneurysms rupture at about 1-2% per year but varies with the size, location and history of previous aneurysm rupture. Unfortunately, most aneurysms present because they have ruptured. Occasionally, large aneurysms can present with vision changes, pain above and behind the eye, nerve paralysis, localized headache, neck pain, nausea and vomiting, or other neurological symptoms. Fortunately, an increasing number of aneurysms are found pryor to rupturing because CT (computed tomography) and MRI (magnetic resonance imaging) are now used commonly to assess patients with these complaints. These are noninvasive methods a radiologist uses to look at the blood vessels in the head. A physician will determine which is the better option for each patient. MR does not involve radiation or contrast risks, while a CT produces better resolution and is better for operative planning. Patients suspected of having a ruptured aneurysm typically undergo a CT scan of the head and a CT angiogram, which shows subarachnoid hermorrhage and the aneurysm.
While CT and MR can show many aneurysms, most patients with aneurysms need a cerebral angiogram for definitive diagnosis and to determine the best treatment. An angiogram is an invasive procedure during which a neuro-interventional surgeon guides a flexible tube (catheter) through an artery over the hip to the vessels of the brain. A liquid dye or contrast agent is injected into the vessel, and pictures are taken with a fluoroscope. An angiogram gives the highest detailed pictures of the location, size, and shape of the aneurysm. All of this information is used to develop the best treatment option for each patient.
Treatment
Not all aneurysms need to be treated and your physician may elect to closely observe your aneurysm. There are two main treatment options for patients who need to have their aneurysm treated.
- Open surgical clipping
- Endovascular therapy: coiling
You physician will discuss these options with you.
Open surgical "clipping":
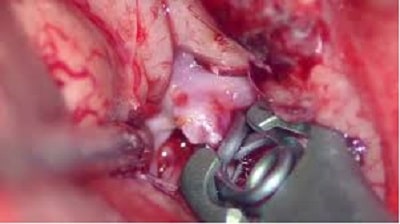 The "open surgical clipping" is performed by a neurosurgeon who will make an incision in the skin over the head, make an opening in the bone and dissect through the spaces of the brain to place a clip accross the aneurysm where it arises from the blood vessel. This prevents the blood flow from entering the aneurysm. Most elective patients spend 2-3 nights in the hospital and then will go home on light restricted activity for 1-2 months after surgery.There have been considerable advances in open surgery techniques. Many neurosurgeons can now perform mini craniotomies, or eye brow incisions to clip an aneurysm. In select patients a small incision is made over the eyebrow. A small two inch window is then made in the bone over the eye and through this incision a small clip is placed across the opening of the aneurysm. These patients usually spend 1-2 days in the hospital after surgery and then go home. Patients are usually on light restricted activity for 1-2 months after surgery. However, it is still an invasive procedure and takes longer to recover from than a coiling procedure.
The "open surgical clipping" is performed by a neurosurgeon who will make an incision in the skin over the head, make an opening in the bone and dissect through the spaces of the brain to place a clip accross the aneurysm where it arises from the blood vessel. This prevents the blood flow from entering the aneurysm. Most elective patients spend 2-3 nights in the hospital and then will go home on light restricted activity for 1-2 months after surgery.There have been considerable advances in open surgery techniques. Many neurosurgeons can now perform mini craniotomies, or eye brow incisions to clip an aneurysm. In select patients a small incision is made over the eyebrow. A small two inch window is then made in the bone over the eye and through this incision a small clip is placed across the opening of the aneurysm. These patients usually spend 1-2 days in the hospital after surgery and then go home. Patients are usually on light restricted activity for 1-2 months after surgery. However, it is still an invasive procedure and takes longer to recover from than a coiling procedure.
Endovascular "coiling"
Endovascular treatment is performed by a neurointerventional surgeon who may be a neuroradiologist, neurosurgeon, or neurologist that has completed additional training. Studies have shown that patients with a ruptured aneurysm tend to do better in the long term after a coiling procedure. A coiling procedure is performed as an extension of the angiogram. A catheter is inserted into a vessel over the hip and other catheters are navigated through the blood vessels to the vessels of the brain and into the aneurysm. Coils are then packed into the aneurysm up to the point where it arises from the blood vessel, preventing blood flow from entering the aneurysm. Most elective patients will go home the next day after surgery and are back to normal activities the following day. More than 125,000 patients worldwide have been treated with detachable platinum coils. Learn more about the development of detachable platinum coil technology.Additional devices, such as a stent or a balloon, may be needed to help keep the coils in place inside the aneurysm. Stent assisted coiling involves permanently placing a stent in the vessel adjacent to the aneurysm to provide a scaffolding of support that keeps the coils within the aneurysm sac. Balloon remodeling involves temporarily placing a removable balloon adjacent to the aneurysm while coils are positioned in the aneurysm.There have been considerable advances in endovascular techniques over the last few years and the field continues to evolve. Most notable is the use of new flow diverting embolization devices. These devices are similar to a stent in that they are placed into the main vessel adjacent to an aneurysm. These devices divert flow away from the aneurysm and provide a scaffolding for healing of the vessel wall to occur. Over time, the aneurysm disappears. This technology allows your doctor to treat many aneurysms that were previously considered untreatable or that were considered to be high risk by other methods. There are many other new devices that are becoming available as well, such as newer that are easier and safer to deliver, as well as stents that can bridge two vessels.
Which procedure should I have?
Both open surgery and endovascular methods are effective. The best treatment for you depends on a number of factors: whether your aneurysm has ruptured, it's size, shape and location. Like all medical decisions, the best treatment option should be made with your physician.




