Piriformis syndrome, hip muscle spasm due to pressure on the sciatic nerve
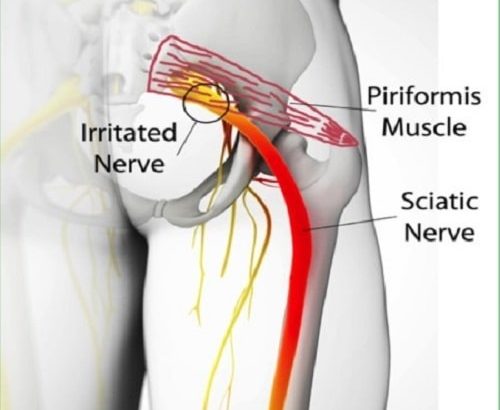
The piriformis muscle, a flat, band-like structure located near the top of the hip joint in the buttocks, is involved in significant lower body movement, and used extensively in sports such as running and biking. It overlies the sciatic nerve, the long main nerve that extends down the back of the leg. The sciatic nerve branches out into smaller nerve endings in the feet. The sciatic nerve innervates the hamstring muscles and all of the muscles below the knee. It also provides feeling to the feet. Nerve compression can occur from spasm of the piriformis muscle or from an odd anatomic structure of the muscle. Piriformis syndrome is characterized by pain, tingling, numbness and weakness of the leg and foot. Approximately 6% of lower back pain and sciatica cases seen in a general practice may be caused by piriformis syndrome.
The piriformis syndrome is a neurological injury. While runners and other professional athletes are typically most familiar with piriformis syndrome, this condition can also affect non-athletes and is usually treatable. Although most cases of sciatica are not the result of piriformis syndrome, long-term treatment depends upon a comprehensive and accurate diagnosis.
cause of Piriformis syndrome
Tension and tightness in the piriformis muscle can cause the muscle to spasm. Like muscle tension in other areas of the body, the causes vary.
Causes can include:
- an injury, such as a fall, a blow to the area, or a car accident
- overuse, such as from frequent running, excessive exercise, or over-stretching
- changing from a sedentary lifestyle to more frequent exercise
- buttock muscles wasting away
- muscle tension and excess weight due to pregnancy
What are piriformis syndrome symptoms?
 There are two main symptoms that can point you towards a piriformis syndrome. We’ll discuss both of them and explain why they appear.
There are two main symptoms that can point you towards a piriformis syndrome. We’ll discuss both of them and explain why they appear.
The first and most pronounced symptom is buttocks pain. The pain is caused by overuse of your piriformis muscle. This overuse damages the muscle, causing it to tighten.
Because the piriformis muscle tightens, it puts pressure on the sciatic nerve. This nerve runs below the piriformis muscle. The pressure causes irritation of the sciatic nerve. This irritation causes a radiating pain at the back side of your leg. This pain can go down your leg as far as your calf muscle. This is the second sign you can recognize a piriformis syndrome of.
This is why it sometimes looks like a herniated disc.
sometimes it even radiates to your back causing lower back pain.
Also, piriformis syndrome reduces your ability to walk, sit for a long period of time and to bend forward to pick something up.
Risk Factors?
There are various risk factors that may make individuals more likely to develop piriformis syndrome.
- Some studies suggest that piriformis syndrome is more common in females by a 6:1 ratio, thought to be due to anatomical differences.
- Anatomical variation in the positioning of the sciatic nerve in relationship to the piriformis muscle may lead to piriformis syndrome. In some people, the sciatic nerve traverses through the piriformis muscle, for example, perhaps increasing the likelihood of sciatic nerve compression.
- Prolonged sitting may lead to direct compression against the sciatic nerve. Piriformis syndrome has, therefore, sometimes been referred to as "fat wallet syndrome" or "wallet sciatica," as it has been found to occur in people continually sitting against their wallet on a hard surface.
Diagnosis
Piriformis syndrome is a somewhat controversial diagnosis. Doctors have argued that it is both under- and over-diagnosed. The controversy is mainly due to a lack of scientifically validated tests.
Many doctors diagnose piriformis syndrome based on symptoms alone. Only two tests that are available can boast significant evidence to support their use. These tests are:
- Magnetic resonance neurography
This form of magnetic resonance imaging (MRI) test looks for inflammation in the nerves.
- FAIR Test
The flexion, adduction, and internal rotation test flexes the hip to stretch the piriformis and compress the sciatic nerve. It measures delays in sciatic nerve signals due to its compression under the piriformis.
treatment

Piriformis syndrome can cause intense pain and may hinder you from engaging in your daily routine. However, you do not have to accept pain or other symptoms as an unalterable aspect of your life. There are various ways to reduce the pain and treatment of this disease that can be effective. These are:
Surgical Solution
For some patients surgical release of the piriformis muscle is often recommended and has been reported to be effective in relieving the symptoms. Surgical decompression through a limited muscle-splitting approach has been used with good or excellent results in 80% of patients.
When non-operative treatment has been exhausted, patients may qualify for operative intervention, which involves decompression of the sciatic nerve in the buttocks. This can often be performed as a day procedure (without overnight stay) and with the aid of an endoscope. In the right population, it can be extremely effective in mitigating piriformis syndrome.
Medication
Oftentimes, anti-inflammatory medications can lessen the effects of piriformis syndrome. Localized injections of pain-relieving medications may also significantly reduce the amount of discomfort experienced by a patient for as long as 6 months, in which time the patient’s case of piriformis syndrome may be resolved through other treatments.
Physical Therapy
By guiding the body through specialized exercises and performing therapeutic massage, physical therapists can sometimes manipulate the piriformis muscle into its proper place while reducing swelling and pain. Other physical therapy modalities, such as heating and cooling treatments, can also yield positive results for patients facing piriformis syndrome.
Injection
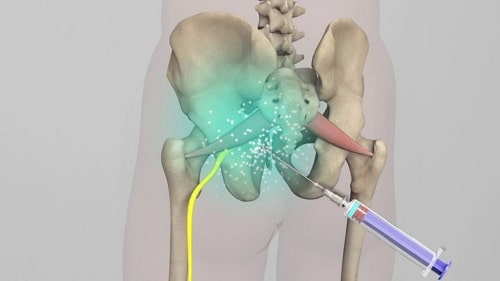
A piriformis syndrome injection can be performed when conservative treatments such as physical therapy fail.
In a study performed with 10 patients with piriformis syndrome, the injection showed good to very good results.
However, it’s also known that these kind of injections may sort only a short time effect. The study group of only 10 is to small to rule this effect out.
Stretches and exercises

A number of stretches and exercises can strengthen the piriformis muscle. Doing these exercises and stretches may help reduce the severity of muscle spasms and relieve muscle tightness.
People with piriformis syndrome may wish to try one or more of the following:
- Lie on the back with the legs extended out. Lift the painful leg toward the chest by holding the knee and ankle. Pull the knee toward the ankle on the other side of the body until a stretch occurs.
- Lie on the back with legs flat and extended. Lift the painful leg and put the foot on the floor on the outside of the opposite knee. Pull the leg across the body with the assistance of a hand, exercise band, or towel.
- With the affected leg crossed over the opposite knee and both legs bent, lie on the back. Pull the lower knee toward the shoulder until a stretch occurs.
Each stretch should be held for 30 seconds and repeated three to five times.
No one should ever force a stretch or perform one that is painful.
Electrotherapy
Your doctor may suggest that you apply electrical stimulation (electrotherapy) to your buttock, which can both reduce muscle spasms related to piriformis syndrome and decrease your experience of pain.
2 common options for electrotherapy are Transcutaneous Electrical Nerve Stimulation units (TENS) and interferential current stimulators (IFC). The difference between the 2 options is that an IFC stimulator penetrates the skin more deeply than a TENS unit, with the added benefit of less discomfort for a given level of stimulation.
Both options may be purchased for long-term use, so you can find relief from the comfort of your home or office. However, before buying any electrotherapy unit a good rule of thumb is to try out an electrotherapy session at your doctor’s office to gauge whether or not it is effective in relieving your symptoms.
Massage therapy
No single treatment option works for everyone, but massage therapy is a little-known treatment for piriformis syndrome that may bring you significant relief from your symptoms.
Massage therapy has at least 2 key benefits in relation to piriformis syndrome:
- A massage relaxes your piriformis muscle, which can prevent spasming and reduce the pressure on your sciatic nerve.
- A massage spurs the release of pain-fighting endorphins, which can reduce your experience of pain from piriformis syndrome.
Your doctor will likely recommend neuromuscular massage therapy—which consists of alternating levels of concentrated pressure on your piriformis muscle.
To find a qualified massage therapist in your area, start by asking your doctor if she or he has any recommendations.
Life Adjustments
Even if your case of piriformis syndrome has cleared, it is important to prevent future episodes by exercising an appropriate amount and evading situations that may aggravate the piriformis muscle. Sitting or lying down for long periods of time, as well as improperly lifting heavy objects, may cause piriformis syndrome to become worse or resurface.
How long does piriformis syndrome last?
Your piriformis syndrome can last for several months if you don’t treat it the right way. However, if you use the exercises we’ll describe later, it will only last for about 4 weeks.
In some severe cases, even with the right exercises it can take months to heal. This is usually because the piriformis syndrome is an outcome of another, bigger problem. In those cases you’ll have to solve the main problem before you can cure your piriformis syndrome.
Prognosis
The prognosis for piriformis syndrome varies, often depending on when it is diagnosed. Since it is a condition that is often overlooked and misdiagnosed, delayed diagnosis is common. Generally speaking, individuals who are diagnosed earlier on in the course of the condition have a better prognosis and respond more favorably to conservative treatment. Those individuals who are not diagnosed in a timely manner may develop chronic piriformis syndrome, which can be more challenging to treat.
Prevention
The same stretches that help with piriformis pain can also reduce the risk of developing piriformis pain.
Many people develop piriformis syndrome due to repetitive movements. Developing good technique can prevent these repetitive motions from damaging the piriformis.
Investing in comfortable, well-fitting running shoes is important. Shoes should ensure that a person moves properly and should not pinch or hurt in other ways. Ill-fitting shoes can undermine posture and form.
Other strategies for prevention include:
- warming up before each workout
- avoiding exercise that causes pain
- treating any injuries promptly
- avoiding exercise using injured muscles until they have healed
- practicing good posture
Piriformis Syndrome During Pregnancy
 What happens with piriformis syndrome is that the pregnant woman begins to secrete the hormone “relaxin” which increases pelvic stretch and can potentially open up the space in the sacro-iliac joints.
What happens with piriformis syndrome is that the pregnant woman begins to secrete the hormone “relaxin” which increases pelvic stretch and can potentially open up the space in the sacro-iliac joints.
Her spine also increases in lordosis (the curvature going anterior), which tilts the pelvis forward, moving it into increased flexion. These things combined cause the gluteal muscle group of the hip/pelvis to become elongated and strained, especially the deep, small muscles of the hip… including piriformis.
Although the occurrence of piriformis syndrome isn’t readily eliminated due to the physiological and postural/biomechanical aggravating factors during pregnancy, massage therapy can be used as a preventative measure and to relieve symptoms when aggravated.




