Arteriovenous fistulas
An arteriovenous fistula, or AVF, is an abnormal connection of vessels in the tissues around the brain or spinal cord in which one or more arteries are directly connected to one or more veins or venous spaces called sinuses. Arteries carry blood from the heart to the tissues, and veins take blood back from the tissues to the heart. In an AVF, there is a direct connection between one or more arteries and veins or sinuses which gives rise to many problems. AVFs differ from arteriovenous malformations (AVMs) in that AVMs are found within the tissue of the brain or spinal cord, but AVFs are found in the coverings of the brain or spinal cord, such as the dura mater or arachnoid. The most serious problem associated with AVFs is that they transfer high-pressure arterial blood into the veins or venous sinuses that drain blood from the brain or spinal cord. This results in an increase in the pressure of the venous system around the brain or spinal cord.
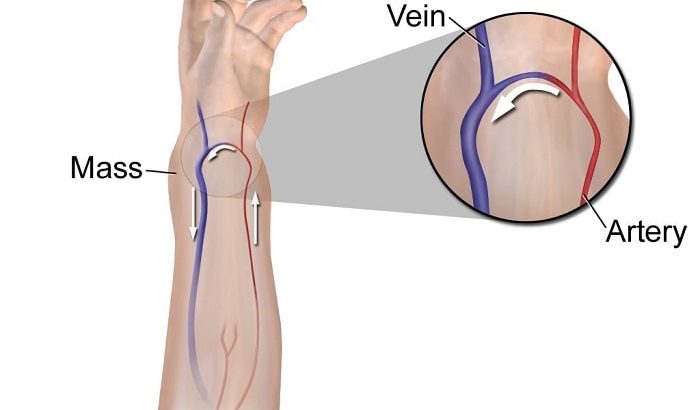
Arteriovenous fistulas can develop anywhere in the body. Arteriovenous fistulas are also often surgically created for use in dialysis in people with severe kidney disease.
A large untreated arteriovenous fistula can lead to serious complications. If you've had an arteriovenous fistula created for dialysis, doctors will monitor you for complications.
Causes of arteriovenous fistulas
 Causes of arteriovenous fistulas include:
Causes of arteriovenous fistulas include:
Cardiac catheterization
An arteriovenous fistula may develop as a complication of a procedure called cardiac catheterization. During cardiac catheterization, a long, thin tube called a catheter is inserted in an artery or vein in your groin, neck or arm and threaded through your blood vessels to your heart.
If the needle used in the catheterization crosses an artery and vein during your procedure, and the artery is widened (dilated), this can create an arteriovenous fistula. This rarely happens.
Injuries that pierce the skin
It's also possible to develop an arteriovenous fistula after a piercing injury, such as a gunshot or stab wound. This may happen if your wound is on a part of your body where a vein and artery are side by side.
Being born with an arteriovenous fistula
Some people are born with an arteriovenous fistula (congenital). Although the exact reason why isn't clear, in congenital arteriovenous fistulas the arteries and veins don't develop properly in the womb.
Genetic conditions
Arteriovenous fistulas in the lungs (pulmonary arteriovenous fistulas) can be caused by a genetic disease (Osler-Weber-Rendu disease, also known as hereditary hemorrhagic telangiectasia) that causes blood vessels to develop abnormally throughout your body, but especially in the lungs.
Surgical creation (AV fistula procedure)
People who have late-stage kidney failure may also have an arteriovenous fistula surgically created to make it easier to perform dialysis. If a dialysis needle is inserted into a vein too many times, the vein may scar and be destroyed.
Creating an arteriovenous fistula widens the vein by connecting it to a nearby artery, making it easier to insert a needle for dialysis and causing blood to flow faster. This AV fistula is usually created in the forearm.
Symptoms
 Small arteriovenous fistulas in your legs, arms, lungs, kidneys or brain often won't have any signs or symptoms and usually don't need treatment other than monitoring by your doctor. Larger arteriovenous fistulas may cause signs and symptoms.
Small arteriovenous fistulas in your legs, arms, lungs, kidneys or brain often won't have any signs or symptoms and usually don't need treatment other than monitoring by your doctor. Larger arteriovenous fistulas may cause signs and symptoms.
Arteriovenous fistula signs and symptoms may include:
- Purplish, bulging veins that you can see through your skin, similar to varicose veins
- Swelling in the arms or legs
- Decreased blood pressure
- Fatigue
- Heart failure
When to see a doctor
If you have any of these signs and symptoms, and think you might have an arteriovenous fistula, make an appointment to see doctor. Early detection of an arteriovenous fistula may make your condition easier to treat and may reduce your risk of developing complications, such as blood clots or, in severe cases, heart failure.
complications of arteriovenous fistulas
Left untreated, an arteriovenous fistula can cause complications, some of which can be serious. These include:
Heart failure
This is the most serious complication of large arteriovenous fistulas. Since your blood flows more quickly through an arteriovenous fistula than it would if your blood flowed through a normal course of arteries, capillaries and veins, your heart pumps harder to compensate for the drop in blood pressure (called high output heart failure). Over time, the increased intensity of your heart's pumping can weaken your heart muscle, leading to heart failure.
Blood clot
An arteriovenous fistula in your legs can cause blood clots to form, potentially leading to deep vein thrombosis, a painful and potentially life-threatening condition if the clot travels to your lungs (pulmonary embolism). Depending on where your fistula is, it can lead to a stroke.
Leg pain
An arteriovenous fistula in your leg can also cause you to develop pain in your legs (claudication), or can worsen pain you already have.
Bleeding
Arteriovenous malformations may lead to bleeding, including into your gastrointestinal system.
Diagnosis
 To diagnose an arteriovenous fistula, your doctor will use a stethoscope to listen to the blood flow through the area where he or she thinks you may have a fistula. The blood flow through an arteriovenous fistula makes a sound similar to clicking or humming machinery (machinery murmur).
To diagnose an arteriovenous fistula, your doctor will use a stethoscope to listen to the blood flow through the area where he or she thinks you may have a fistula. The blood flow through an arteriovenous fistula makes a sound similar to clicking or humming machinery (machinery murmur).
If your doctor hears a machinery murmur, you'll have other tests to confirm that the murmur is caused by an arteriovenous fistula. These can include:
Duplex ultrasound
Duplex ultrasound is the most effective and common way to check for an arteriovenous fistula in the blood vessels of your legs or arms. In duplex ultrasound, an instrument called a transducer is pressed against your skin over the suspicious area.
The transducer produces high-frequency sound waves, which bounce off red blood cells. A duplex ultrasound can estimate how fast blood flows by measuring the rate of change in its pitch (frequency).
Computerized tomography (CT) angiogram
A CT angiogram allows your doctor to check your arteries to see if blood flow is bypassing the capillaries. You'll receive an injection of a dye that shows up on CT images, and the doughnut-shaped CT scanner will be moved to take images of the artery your doctor believes is narrowed. The images are then sent to a computer screen for your doctor to view.
Magnetic resonance angiography (MRA)
Your doctor may use an MRA if he or she thinks you may have an arteriovenous fistula in an artery that's deep under your skin. This test allows your doctor to see the soft tissues in your body. It uses the same technique as magnetic resonance imaging (MRI), but also includes the use of a special dye that helps create images of your blood vessels.
During an MRI or MRA, you lie on a table inside a long tube-like machine that produces a magnetic field. An MRI machine uses the magnetic field and radio waves to create pictures of your body's tissues. Using the images from the test, your doctor may be able to see an arteriovenous fistula.
treatment
It's possible your doctor may suggest only monitoring your arteriovenous fistula, especially if it's small and doesn't cause any other health problems. Some small arteriovenous fistulas close by themselves without treatment.
If your arteriovenous fistula requires treatment, your doctor may recommend:
Surgery
The surgery treatment that doctor recommends will depend upon the circumstances of your arteriovenous fistula and your health history, but it will generally be one of two types of surgery: catheter embolization or microsurgical resection.
The treatment goal of both procedures is generally the same: Stop blood from flowing through the arteriovenous fistula, which is a malformation of the circulatory system.
Catheter Embolization
One treatment option is called catheter embolization. The neurosurgeon makes an incision near the groin, in the upper inner thigh, to access an artery, then inserts a catheter. He will use an imaging-guided system to direct the catheter to the site of the arteriovenous fistula. Then he will inject a material called an embolic agent, which essentially stops up the blood vessel and blocks the blood from flowing through the malformed area. The embolic agent might be a glue-like material or something called Onyx. During this procedure for arteriovenous fistula repair, you will usually be under general anesthesia to maximize your comfort and allow the neurosurgeon to perform the surgery.
Recovering From Catheter Embolization
Your recovery from a catheter embolization begins in the hospital, where you can expect to stay for a day or two after the procedure. Right after the procedure, you may be asked to lie flat for about six hours, but after that you may sit up and walk if you feel ready. During this time, your doctor will be monitoring your incision for bleeding or swelling and checking for any complications from the embolization procedure itself.
Recovering at home can take anywhere from a few days to a few weeks, depending on your overall health and other factors. In the early days of your recovery, activities like driving, exercise and heavy lifting will be restricted, and it’s important to get plenty of rest. Your doctors may prescribe medications for pain and other issues. You will need to check the incision site at your inner thigh for signs of infection and bleeding, although this incision site typically is without complication.
You can gradually resume normal activities over the next week or so.In the weeks after catheter embolization, you can expect to see your doctors for a follow-up to check the healing of your incision and the outcome of the procedure. Some people also needed multiple embolization procedures spread over time, something called staged embolization.
This procedure is considered minimally invasive and is a means for the neurosurgeon to indirectly access the arteriovenous fistula. However, it is not appropriate for all patients, as some arteriovenous fistulas cannot be closed up using an embolic agent.
Microsurgical Resection
Some patients are not good candidates for catheter embolization, so your physician may recommend a different procedure for arteriovenous fistula repair, called microsurgical resection. Microsurgery is surgery done under a special microscope, which allows the surgeon to have greater visibility while performing delicate procedures. Because of this cutting-edge technology, cerebrovascular neurosurgeons can perform surgeries that were previously too difficult, or even impossible, to undertake.
During this procedure, your neurosurgeon will directly access your arteriovenous fistula to repair it. The neurosurgeon will need to perform a craniotomy in order to access the blood vessels. This means that they will remove a small section of the skull, providing them with direct access to the site of malformation.
However, not all patients will need to undergo a craniotomy, depending upon the location and circumstances. Not all atrioventricular fistulas occur around the brain, and even some that do can be accessed through incisions at other sites. Like catheter embolization, microsurgical resection requires you to be under general anesthesia.
Recovering From Microsurgical Resection
Your recovery from microsurgery to remove an AVF depends on many factors, including your age, health, and the location and size of the fistula. Generally, though, you can expect to spend about three to five days in the hospital while your care team monitors your recovery from anesthesia and the healing of your incision and checks for any complications from the procedure.
Recovering at home can take several weeks, usually six weeks, but your recovery will vary due to your health and circumstances, as all patients are different. Your doctors will provide specific instructions on caring for your incision after you go home. You can expect to have restrictions on driving, lifting and strenuous activities for a week or so, with a gradual return to normal activities over the next few weeks.
During this time, you may feel fatigued and have some pain, so your doctors may prescribe medications to help your recovery. If your surgery involved the brain, you may have temporary neurological problems, such as difficulty concentrating or problems with coordination or balance. In the weeks after surgery, you can expect to see your doctors for follow-ups to remove stitches and check the progress of your healing. You can expect to be back to work after six weeks.
Ultrasound-guided compression
If you have an arteriovenous fistula in your legs and it's easily visible on ultrasound, treatment with ultrasound-guided compression may be an option for you. In this treatment, an ultrasound probe is used to compress the fistula and block blood flow to the damaged blood vessels.
This procedure only takes about 10 minutes. But it only works for about one in three people.




